On July 26, 2013, the Department of Justice announced the settlement with Dubuis Health System. Dubuis operates long-term acute care hospitals in a number of states located in the Southern East and South Western United States. The health system does not operate any facilities in the state of New Jersey.
A former Administrator at Southern Crescent (part of the health system) alleged that the health system kept patients hospitalized beyond what should have been considered “medically necessary”. The health system did this for two reasons; the system would receive a higher rate of Medicare reimbursement and, the health system could maintain its classification as a long-term acute care facility.
It was alleged that the fraud occurred between 2003 and 2009. It is not known whether or not there were allegations before or after these dates of fraud.
The health system agreed to pay $8 million to resolve the allegations. The whistleblower will receive a little more than $2.1 million of the recovery by the United States government.
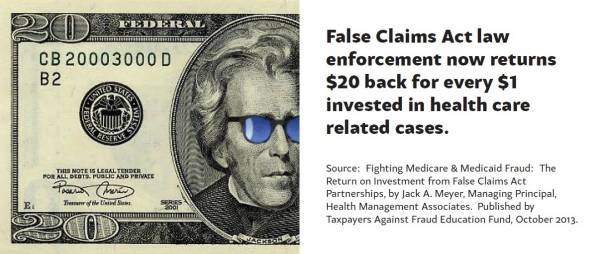
Healthcare fraud, including long-term acute care facilities, nursing homes, and hospice has been a hot topic over the last number of years. The False Claims Act, a federal statute, has provided a vehicle for the federal government to become aware of the fraud. Very often, the fraud is not known to the federal government and is brought to the attention of the Department of Justice by an individual. The individual can be an employee, a competitor, or, in some cases, a patient. The individual that brings the fraud to the attention of the federal government is called a “relator”. The False Claims Act provides for the relator to receive an award based upon the success of the case. The False Claims Act is very particular and has significant requirements including the need for the information to not have been public and the relator must be the first person to bring the information to the attention of the federal government. For this reason, relators often seek the services of a whistleblower lawyer with experience in the area. The False Claims Act provides for an award of between 15% and 30% of the amount recovered by the federal government.
Although this healthcare system did not maintain facilities in the state of New Jersey, if New Jersey had paid any of the bills which were improper, there would have been a recovery for the state of New Jersey as well. This is due to the fact that the state of New Jersey passed a False Claims Act in 2008. The New Jersey False Claims Act, very similar to the Federal False Claims Act, provides for a vehicle to report fraud against the state of New Jersey or state authorities.
Continue reading
 New Jersey Whistleblower Lawyer Blog
New Jersey Whistleblower Lawyer Blog